![]()
News release from the National Institutes of Health:
Drug boosts growth factor to jump-start rapid antidepressant response
Little-known enzyme pivotal — NIH-funded study in mice
A study in mice has pinpointed a pivotal new player in triggering the rapid antidepressant response produced by ketamine. By deactivating a little-known enzyme, the drug takes the brakes off rapid synthesis of a key growth factor thought to lift depression, say researchers supported by the National Institutes of Health.
“Other agents that work through this pathway and block the enzyme may also similarly induce anti-depressant-like effects and hold promise for development of new treatments,” said Lisa Monteggia, Ph.D., of the University of Texas Southwestern Medical Center, Dallas, a grantee of the NIH’s National Institute of Mental Health.
Monteggia, Ege Kavalali, Ph.D., and colleagues reported their findings online June 15, 2011 in the journal Nature.
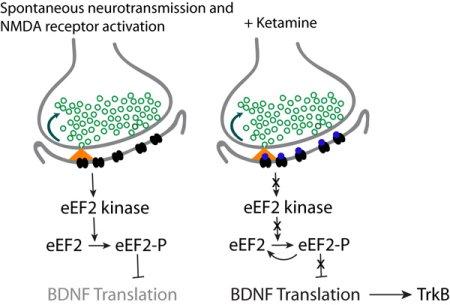
When in their default (resting) state, neurons that mediate ketamine’s action engage in the brain’s equivalent of background chatter. They spontaneously spray out (orange) the chemical messenger glutamate (green circles), which binds to NMDA receptors (black ovals) on adjoining neurons. This activates the enzyme eEF2 kinase, which suppresses synthesis of BDNF, a growth factor that has antidepressant effects. Treatment with ketamine blocks the binding of the neurotransmitter to the receptors (blue dots on black ovals), which inactivates the enzyme, taking the brakes off translation of BDNF into protein. This jump-starts a fast-acting antidepressant effect. Source: Lisa Monteggia, Ph.D., University of Texas Southwestern Medical Center.
Unlike currently available antidepressants that take weeks to work, ketamine can lift mood within hours. Yet adverse side effects of this animal anesthetic — and sometime club drug — preclude it from becoming a practical treatment. So researchers have been studying its mechanism of action, in hopes of developing safer alternatives that work the same way.
Earlier studies had shown that the growth factor, called brain-derived neurotrophic factor (BDNF), produces antidepressant-like effects. To find out if BDNF is involved in ketamine’s action, the researchers gave the drug to mice genetically engineered to lack BDNF. Unlike in control mice, ketamine failed to produce a fast-acting antidepressant-like response in such BDNF knockout mice exposed to experimental situations that trigger depression-like behaviors. This and other tests confirmed that ketamine’s rapid antidepressant effects depend on rapid synthesis of BDNF in the brain’s memory center, or hippocampus.
The researchers determined that this happens so quickly — within 30 minutes — because time-consuming intermediate steps have already been completed. It only requires the translation of BDNF mRNA, an intermediate form, into the final protein. By contrast, conventional antidepressants are thought to work through a much more lengthy and indirect process that requires, among other things, the birth of new neurons and their integration into circuits.
Ketamine achieves this boost in BDNF levels by first blocking a protein on neurons (brain cells) called the NMDA receptor. The Texas team discovered that this blockade, in turn, deactivates an enzyme called eukaryotic elongation factor 2 (eEF2) kinase, which restrains BDNF synthesis. So ketamine (and presumably other agents that similarly turn off the enzyme) effectively takes the brakes off of this antidepressant mechanism.
“Selectively inhibiting the eEF2 kinase was sufficient to trigger a rapidly acting antidepressant response in control mice but not in mice lacking BDNF,” explained Monteggia.
The researchers discovered that the boost in BDNF occurs while neurons are in their default mode – not doing anything in particular. But the cells continue communicating via a low level of background chatter, spontaneously releasing chemical messengers that bind to receptors. So when ketamine blocks NMDA receptors, it prevents their naturally occurring messenger chemical, glutamate, from binding to them.
“Interference with such spontaneous neurotransmission to trigger production of a protein represents a novel mode of drug action,” Monteggia noted. “It may also hold clues to what goes awry in the brain in disorders like depression.”
Although BDNF levels fall off sharply following the transient increase triggered by ketamine, she says evidence may also support a role for BDNF in the drug’s longer-term antidepressant effects. The exact role of another enzyme implicated in ketamine’s antidepressant action remains to be determined, in light of the new findings. Yale researchers reported last fall that the drug triggered increased connections between neurons via effects on the enzyme, called mTOR.
“This discovery of a novel pathway involved in mediating fast-acting antidepressant action holds hope for development of new rapid-acting medications,” said Monteggia.
The mission of the NIMH is to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery and cure. For more information, visit the NIMH website.
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
Reference: NMDA receptor blockade at rest triggers rapid behavioral antidepressant responses. Autry AE, Adachi M, Nosyreva E, Na ES, Los MF, Cheng PF, Kavalali ET, Monteggia LM. Nature. 2011 Jun 15. doi: 10.1038/nature10130. [Epub ahead of print] PMID:21677641